Streptozotocin-Induced Diabetic Neuropathy in Mice and Rats

Induction:
Animals will be injected with streptozotocin (STZ) IP or IV once after fasting for 12-18hrs (animals will have free access to food after STZ administration). The following tables show the dose, route, and duration of the study:
RATS
| STZ Dose (mg/kg) | Duration of Study | Dose Route |
|---|---|---|
| 40-65mg/kg5-8 | Up to 1 week post STZ dose | IV |
| 65-75mg/kg1-4,9,10 | Up to 4 weeks post STZ dose | IP |
MICE
| STZ Dose | Duration of Study | Dose Route |
|---|---|---|
| 150mg/kg11 | Up to 1 week post STZ dose | IV |
| 100-200mg/kg11-15 | Up to 4 weeks post STZ dose | IP |
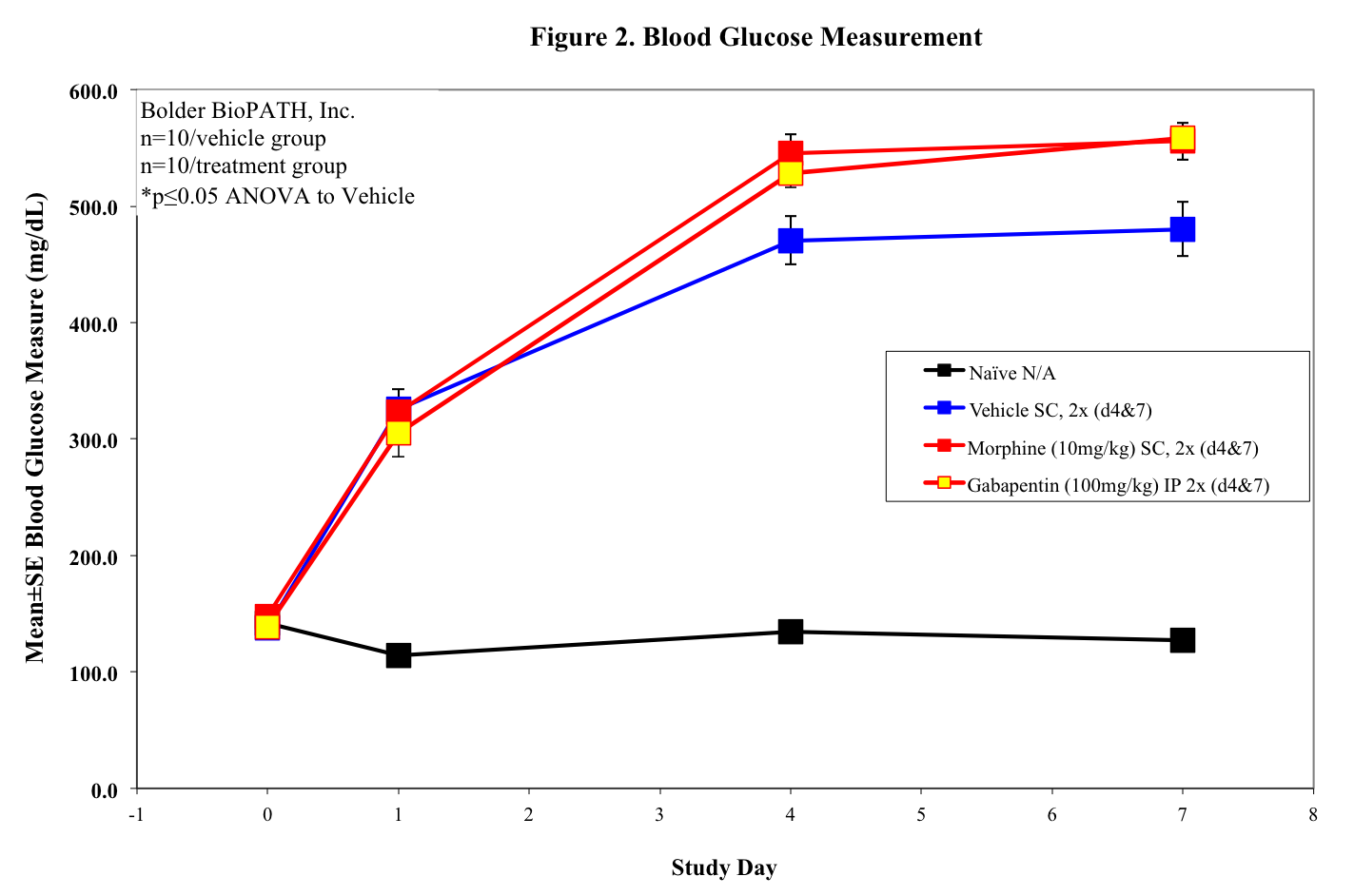
Disease Parameters/Progression:
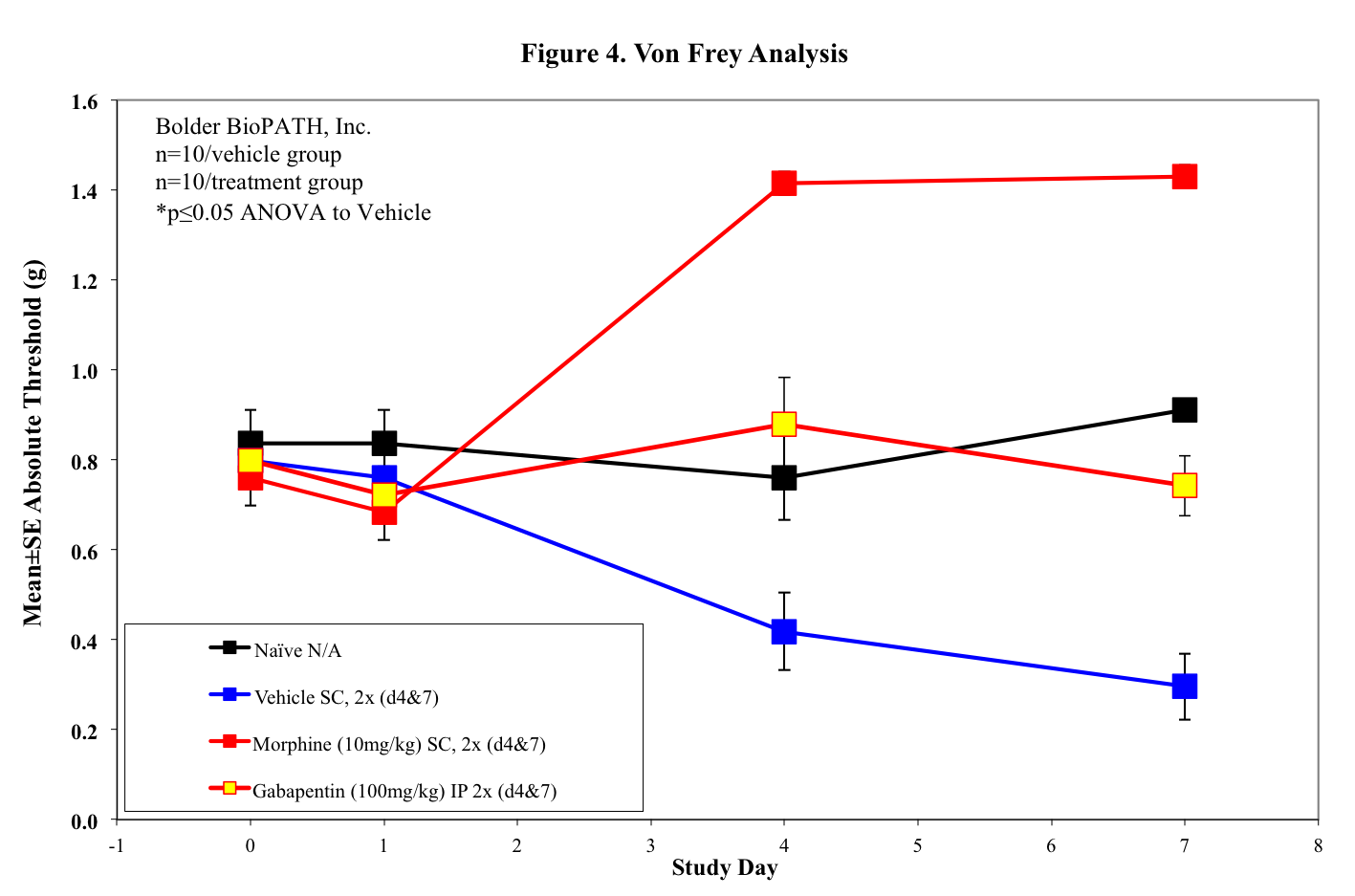
Prior to STZ injection animals will have a glucose test via tail snip and a von Frey baseline. Animals will be fasted for no longer than 18hrs (typically 12-18hrs) before STZ injection. One hour after injection animals will have free access to food. Depending on the duration of the study (acute vs chronic), animals will be enrolled in the study by glucose test to determine hyperglycemia 24 hrs or 7 days post STZ administration. Following enrollment, animals will continue to get glucose tests and von Frey tested for development of neuropathy as necessary (typically weekly testing in chronic studies). Administration of analgesics will only occur on behavior testing days as a control.
Dosing Paradigms:
Route of administration: SC, PO, IP, IV
Clinical Assessment:
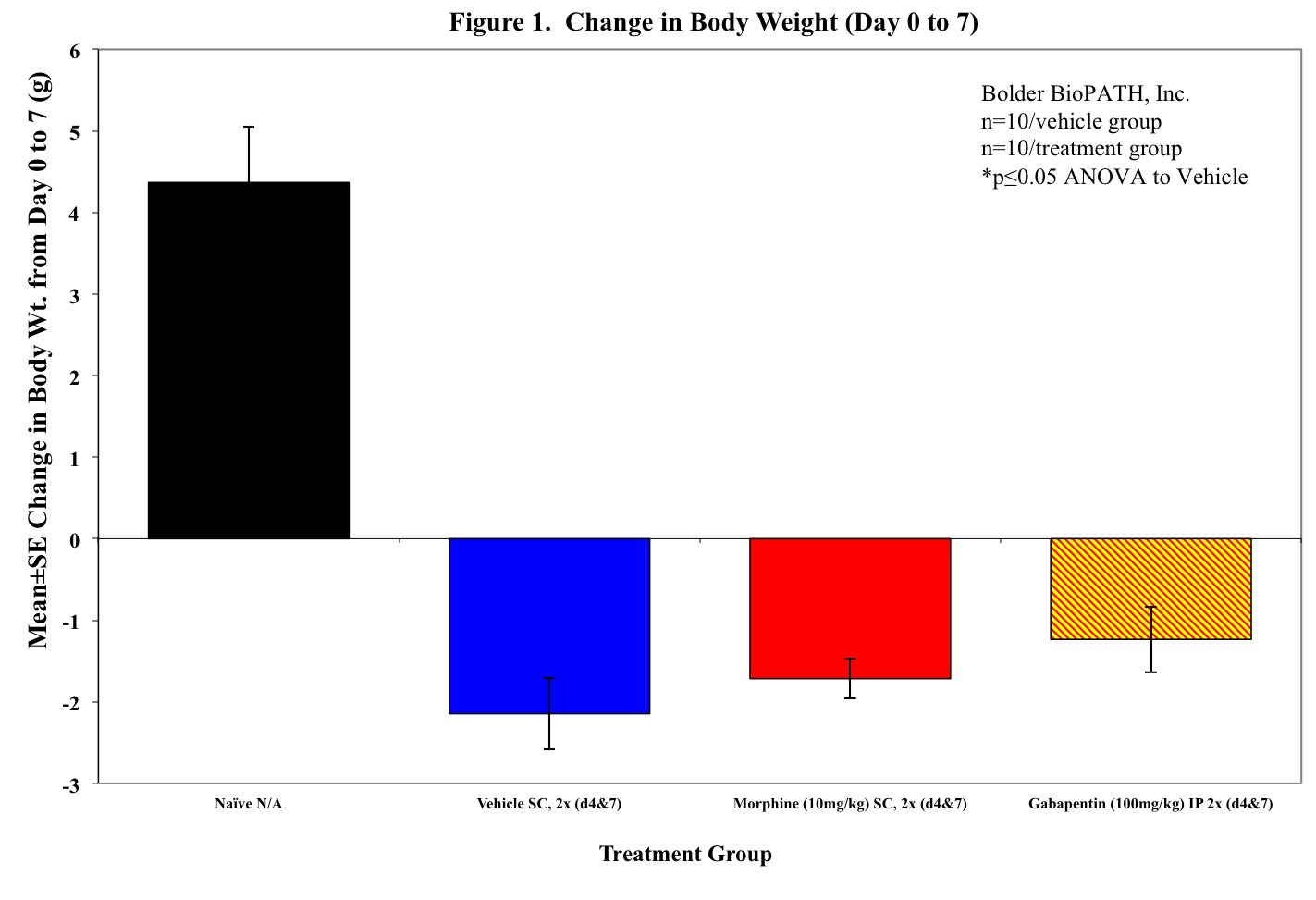
Body weights will be tracked for the duration of the study and von Frey testing will be performed to monitor pain. Depending on the dosing paradigm used, studies may last up to 4 weeks (neuropathy typically peaks 2-4 weeks after IP STZ injection).
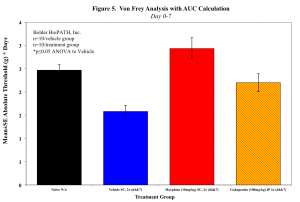
Sample Data (Click on image to enlarge):
Mouse Clinical
Rat Clinical
Pain Data
Notes:
Streptozotocin (STZ) is toxic to pancreatic islet insulin-producing b-cells, thus inducing diabetes. Other models of diabetes include genetic models and the use of a prolonged high-fat diet regimen. The STZ model provides a good, simple screening tool to test compounds and to further understand the complex development of neuropathic pain.
Animals will not be supplemented with insulin, except possibly as a control, since it may hinder the development of STZ-induced neuropathy4,5. Also, rats should be housed no more than 2 per cage and should be changed at least 3 times per week (if in standard housing), as they tend to drink a lot and soil their cage quickly.
Optional Endpoint
- PK/PD blood collections
- Cytokine/chemokine analysis via Luminex(R)
- Other sandwich ELISAs
- CBC/clinical chemistry analysis
- Soft tissue collection
- Histopathologic analysis
- Immunohistochemistry analysis
References
- Ali G, Subhan F, et al. A streptozotocin-induced diabetic neuropathic pain model for static or dynamic mechanical allodynia and vulvodynia: validation using topical and systemic gabapentin. Nauyn-Schmiedeberg’s Arch Pharmacol. 2015; 388:1129-1140.
- Byrne FM, Cheetham S, et al. Characterisation of pain responses in the high fat diet/streptozotocin model of diabetes and the analgesic effects of antidiabetic treatments. J Diabetes Res. 2015; 2015.
- AlSharari SD, Al-Rejaie SS, et al. Ameliorative potential of morin in streptozotocin-induced neuropathic pain in rats. Tropical J of Pharmaceutical Res. 2014; 13(9): 1429-1436.
- Fox A, Eastwood C, et al. Critical evaluation of the streptozotocin model of painful diabetic neuropathy in the rat. Pain. 1999; 81: 307-316.
- Cunha JM, Cunha FQ, et al. Streptozotocin-induced mechanical hypernociception is not dependent on hyperglycemia. Brazilian J of Med and Bio Res. 2009; 42: 197-206.
- Gross ML, El-Shakmak A, et al. ACE-inhibitors but not endothelin receptor blockers prevent podocyte loss in early diabetic neuropathy. Diabetologia. 2003; 46:856-868.
- Pospisilik JA, Martin J, et al. Dipeptidyl peptidase IV inhibitor treatment stimulates b-cell survival and islet neogenesis in streptozotocin-induced diabetic rats. Diabetes. 2003; 52:741-750.
- Junod A, Lambert AE, et al. Diabetogenic action of streptozotocin: relationship of dose to metabolic response. J of Clin Invest. 1969; 48: 2129-2139.
- Fuchs D, Birklein F, et al. Sensitized peripheral nociception in experimental diabetes of the rat. Pain. 2010; 151:496-505.
- Courtiex C, Eschalier Al, and Lavarenne J. Streptozocin-induced diabetic rats: behavioural evidence for a model of chronic pain. Pain. 1993; 53: 81-88.
Related Pages
Pain Models
- Monosodium Urate-Induced Gout (Rat, Mouse)
- Carrageenan Induced Paw Edema (Rat, Mouse)
- Streptozotocin-Induced Diabetic Neuropathy in Mice and Rats
- Rat Partial Sciatic Nerve Ligation
- Bone Tumor Pain
Rheumatoid Arthritis
- Collagen Induced Arthritis (CIA) in Rat
- Strep Cell Wall (SCW) Reactivation Arthritis (PGPS)
- Antigen Induced Knee Arthritis (Mouse)